Starting in January 2019, the Preclusion List from the Centers for Medicare and Medicaid Services (CMS) will be made available to all Medicare Advantage plans and Part D sponsors, and will officially go into effect in April 2019. This new rule has been put into action to replace the Medicare Advantage (MA) prescriber enrollment requirements.
In addition, the list will be used to ensure patient protection and safety, and protect Trust Funds from prescribers and providers who are identified as fraudulent. We’ve taken some time to break down each element of the CMS Preclusion List and what it could mean for your organization. Please take a look and of course, feel free to ask us any questions!
What is the CMS Preclusion List?
The Preclusion List from the Centers for Medicare and Medicaid Services (CMS) is a list of providers and prescribers who are precluded from receiving payment for Medicare Advantage (MA) items and services or Part D drugs furnished or prescribed to Medicare beneficiaries.
Why was the CMS Preclusion List Created?
- To replace the Medicare Advantage (MA) and prescriber enrollment requirements
- To ensure patient protections and safety and to protect the Trust Funds from prescribers and providers identified as bad actors
In the April 2018 release of the Federal Register Rules and Regulations, the Department of Health and Human Services released policy and technical changes to a variety of Medicare programs included in the CMS-4182 Final Rule document.
Who is on the CMS Preclusion List?
The CMS Preclusion List is a list of prescribers and individuals or entities who fall within any of the following categories:
(1) Are currently revoked from Medicare, are under an active re-enrollment bar, and CMS has determined that the underlying conduct that led to the revocation is detrimental to the best interests of the Medicare program.
(2) Have engaged in behavior for which CMS could have revoked the prescriber, individual, or entity to the extent applicable if they had been enrolled in Medicare, and CMS determines that the underlying conduct that would have led to the revocation is detrimental to the best interests of the Medicare program. Such conduct includes, but is not limited to, felony convictions and Office of Inspector General (OIG) exclusions.
How are Providers Notified When They are on the CMS Preclusion List?
CMS will issue an initial email notification to the impacted providers using the email addresses obtained from the Provider Enrollment Chain and Ownership System (PECOS) the Medicare enrollment system of record or the National Provider Plan and Enumeration System (NPPES). The Centers for Medicare and Medicaid Services (CMS) or a Medicare Administrative Contractor (MAC) will follow up with a written notice through the mail to the impacted provider in advance of his or her inclusion on the list and their applicable appeal rights.
How Long Can a Provider Be on the CMS Preclusion List?
A provider will be precluded for the length of their re-enrollment bar if they are currently revoked or would have been revoked had they enrolled in the Medicare program. The re-enrollment bar is a minimum of 1 year, but not greater than 3 years depending on the severity of the basis for revocation. The timeframe will be specified in the notification letter.
How Does the CMS Preclusion List Affect My Organization?
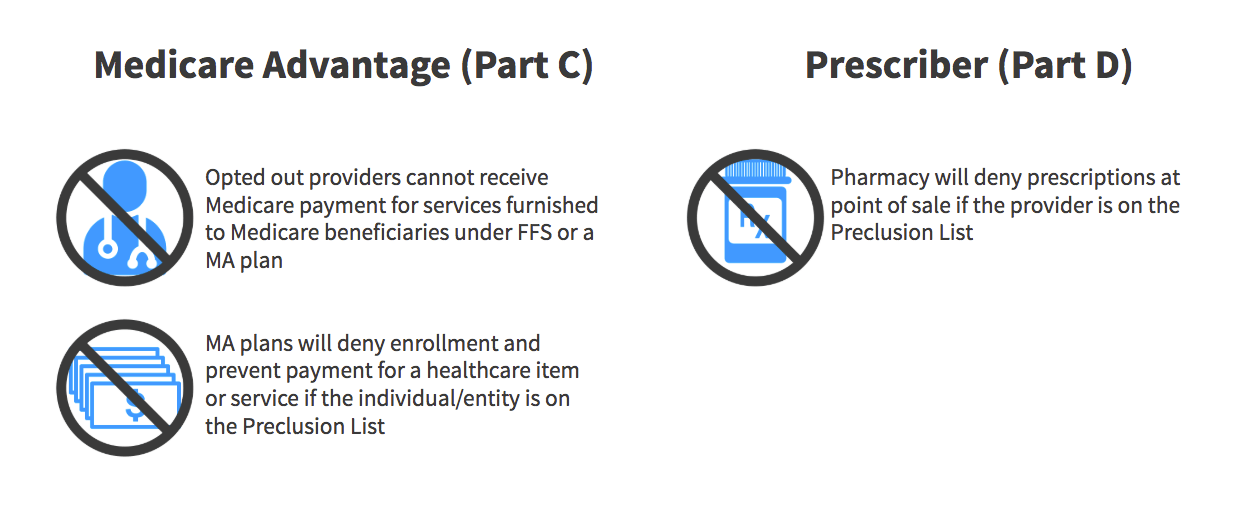
In accordance with this new regulation, Medicare Advantage (MA) Plans will be prohibited from paying for services by providers and suppliers who are named to the Preclusion List, and also requires pharmacy benefit managers to reject a pharmacy claim for a Part D drug if the individual who prescribed the drug is included on the list as determined by the Centers for Medicare and Medicaid Services (CMS).
The new rule aims to allow more flexibility for healthcare providers and suppliers not currently enrolled in Medicare to provide care to Medicare Advantage (MA) members. Also, providers who have chosen to opt out of traditional Medicare are able to prescribe Part D covered drugs or administer care for Part C beneficiaries.
Our team is keeping an eye on new announcements from the Centers for Medicare and Medicaid Services (CMS) for the latest releases and additional information for Medicare Advantage, health systems, health plans, and more! If you have any questions about how to prepare for the CMS Preclusion List, please feel free to comment or contact us – we’d be happy to help!









