While U.S. COVID-19 cases continue to rise, there’s no denying the recent light shed on the disparities in health outcomes for racial and ethnic minority groups and among low-income populations. As more information is gathered on the rates of infection and outcomes for the coronavirus disease (COVID-19), the further we see that there’s a disproportionate burden of infection and deaths among communities of color and those economically disadvantaged.
A data snapshot of the impact of COVID-19 on the Medicare population
The Centers for Medicare & Medicaid Services (CMS) has called for a renewed national commitment to value-based care based on Medicare claims information that provides an early snapshot of the impact of the coronavirus disease 2019 (COVID-19) pandemic on the Medicare population. The results drastically show that racial and ethnic minority groups, low-income populations, and elderly Americans with chronic conditions have the most significant risk of COVID-19.
For Black Americans who have higher rates of underlying conditions, such as diabetes and heart and lung disease, a lack of access to quality healthcare and discrimination or bias has detrimental effects.
CDC Data Collection on Disparities in COVID-19 Cases and Outcomes
The Centers for Disease Control (CDC) has been collecting and maintaining data that can be used to evaluate racial, ethnic, and socioeconomic disparities in COVID-19 cases and outcomes.
HHS OIG presented a new Work Plan item to examine this data collection and review how the CDC uses it to address the COVID-19 pandemic. Furthermore, the HHS OIG will additionally review the CDC’s findings to determine how to adequately protect both communities of color and economically disadvantaged communities in public health emergencies.
A Long History of Racial Disparities in Healthcare
Dr. Utibe Essien, a health equity researcher with the University of Pittsburgh, says, “I think it’s important to appreciate that the pandemic didn’t start something new, but that these disparities really, unfortunately, have been seen for decades, if not centuries.” Evidence of this can be seen here where hospital rankings show ‘elite’ facilities struggle with health equity, inclusivity.
According to CMS, “The disparities in the data reflect long-standing challenges facing minority communities and low income older adults, many of whom face structural challenges to their health that go far beyond what is traditionally considered ‘medical,’” said CMS Administrator Seema Verma. “Now more than ever, it is clear that our fee-for-service system is insufficient for the most vulnerable Americans because it limits payment to what goes on inside a doctor’s office.”
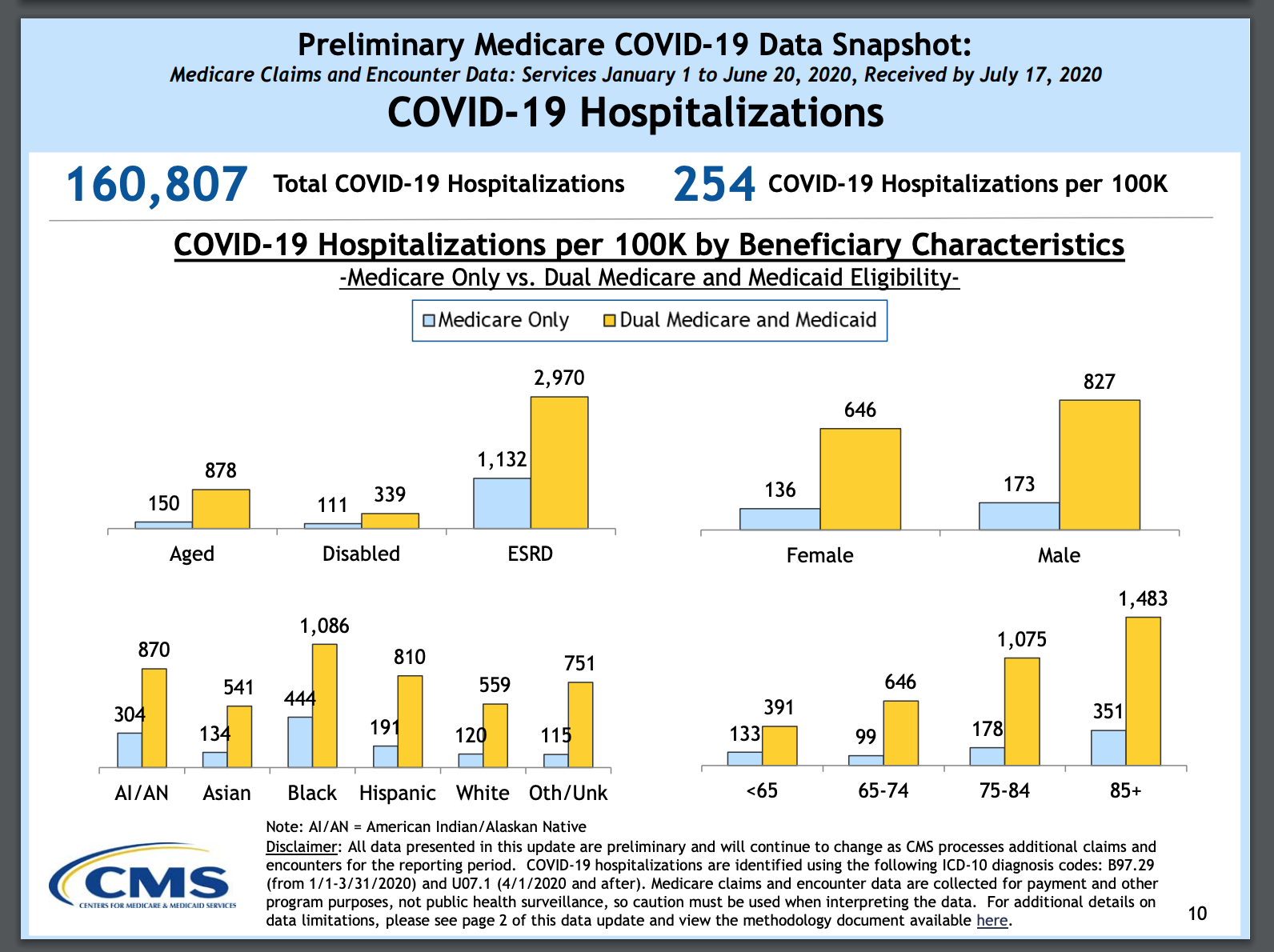
The CMS data released in late June includes the number of reported COVID-19 cases and hospitalizations among Medicare beneficiaries between January 1 and May 16, 2020, plus a snapshot of COVID-19 cases and hospitalizations for Medicare beneficiaries by state, race/ethnicity, age, gender, dual eligibility for Medicare and Medicaid, and urban/rural locations.
The Medicare data also shows that:
- Black Americans with COVID-19 were hospitalized at a rate nearly four times higher than white Americans, with 465 per 100,000 compared to 123 per 100,000 for white Americans. Hispanics had 258 hospitalizations per 100,000, and Asians had 187 per 100,000.
- Black Americans have experienced the highest death rates, with about 88.4 deaths per 100,000, compared to 40.4 per 100,000 for white Americans.
- The rate of COVID-19 cases for dual eligible individuals is higher across all age, sex, and race/ethnicity groups.
Healthcare Fraud and Racial Inequities
The Johns Hopkins Bloomberg School of Public Health created a study that examined providers excluded from Medicare due to fraud and abuse. The study found that the patients who were being treated before the provider was banned were, more likely, minorities, disabled individuals, and those dually-enrolled in Medicaid. These vulnerable patients may have experienced patient neglect, illegally-provided prescriptions, unnecessary medical procedures, deceitful billing practices, and untrained personnel contact.
During the study, the researchers analyzed the demographics of patients seen by excluded and non-excluded providers, considering the patient’s location, age, and the type of provider. They found that not only were more patients more likely to be non-white, 27.4 percent versus 25 percent seen by non-excluded healthcare providers, but they were also more likely to be dually-eligible for Medicaid, 38.8 percent versus 25.5 percent, and non-elderly disabled, 21.6 percent versus 17.3 percent.
Watch this webinar replay to learn more about excluded providers.
Government Responses to Healthcare Racial Inequities and Discrimination
The Centers for Medicare and Medicaid Services
- Planning to increase the implementation of a value-based system that rewards providers for keeping patients healthy and gives consumers information about disease prevention and outcomes needed to help make healthcare choices on the basis of quality.
- Encouraging states to double down on efforts to protect low-income seniors and look at the data and determine what resources are available, both locally and federally, to improve this disparity of health outcomes.
- Identifying a range of operational opportunities for states to improve care for dually eligible individuals and various models that states can participate in that focus on improving the quality and cost of care for individuals who are concurrently enrolled in Medicaid and Medicare.
CMS Office of Minority Health
- Holding a series of listening sessions with key stakeholders responsible for providing care to racial and ethnic minorities.
HHS Office for Civil Rights (OCR)
- Enforcing Title VI, prompting healthcare systems to take action in the hopes of eliminating healthcare disparities.
Center for Medicaid and Children’s Health Insurance Program (CHIP) Services
- Developing guidance for states on new opportunities to adopt innovative, value-based payment design and implement strategies to address social determinants of health for their beneficiaries, including those who are dually eligible for Medicare and Medicaid.
Eliminating Fraud, Waste, and Abuse from Government Health Programs
The spotlight has never been brighter on both the communities most affected by COVID-19 and the gaps in quality of care received from beneficiaries in government health programs. This is imperative in the fight against discrimination and the discontinuation of provider fraud and abuse, which unfortunately target vulnerable minorities, individuals with disabilities, and those dually-enrolled in Medicaid.









