Eliminate Ineligible Claims and Reduce Overpayment
Reduce Overpayment and Wasteful Spending
Overpaying claims and trying to recoup later is inefficient
Claims recovery efforts are costly

Ensure Compliance in a Shifting Regulatory Environment
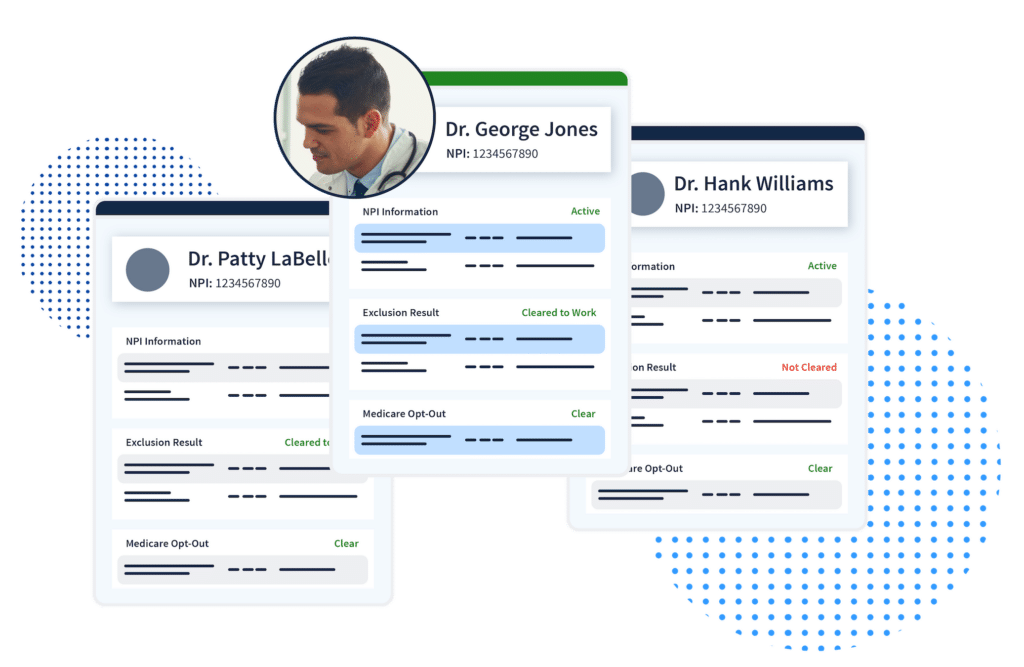
Maintain an up-to-date directory of eligible providers
Defend the integrity of your government LOBs
With monitoring that is both smarter and faster, you can catch exclusions and other issues hiding in your provider network among par and non-par providers alike.
Simplify Administrative Complexities and Workflows
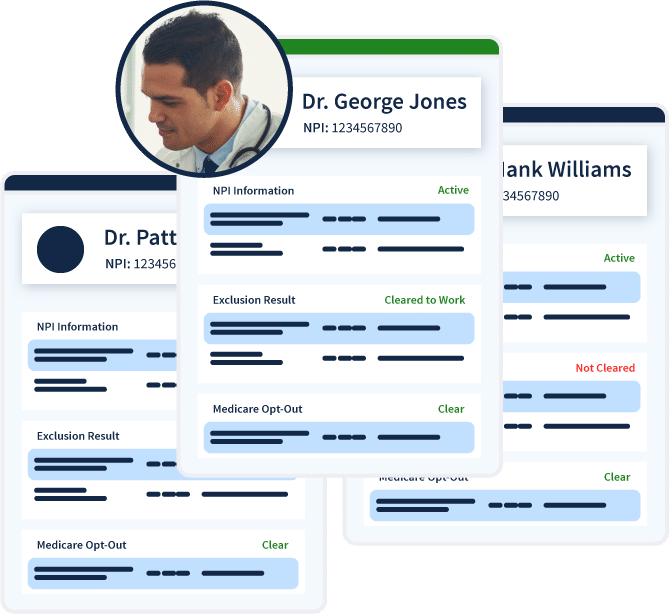
Adjust your claims editing process to include eligibility pre-checks
Why wait until post-payment to identify provider network eligibility? Our always-accurate intelligence provides simplified insights about your provider network, empowering your team to remove bad actors before the claims editing process even begins.
Connect your system of record via seamless and secure integrations
Speed to action is critical for pre-payment screening. We’ve designed our provider network monitoring to deliver fully verified eligibility alerts weeks (or months) before any other solution. Access your provider insights in your system of record through our seamless and secure API integrations.


In a short period of time, ProviderTrust’s guidance and expertise has simplified our day-to-day operations and improved our overall business, but more importantly, it’s allowed us to focus on achieving our mission ‘To Improve the Oral Health of All.'"
Data Accuracy and Integrity Built to Scale
Provider Network Monitoring
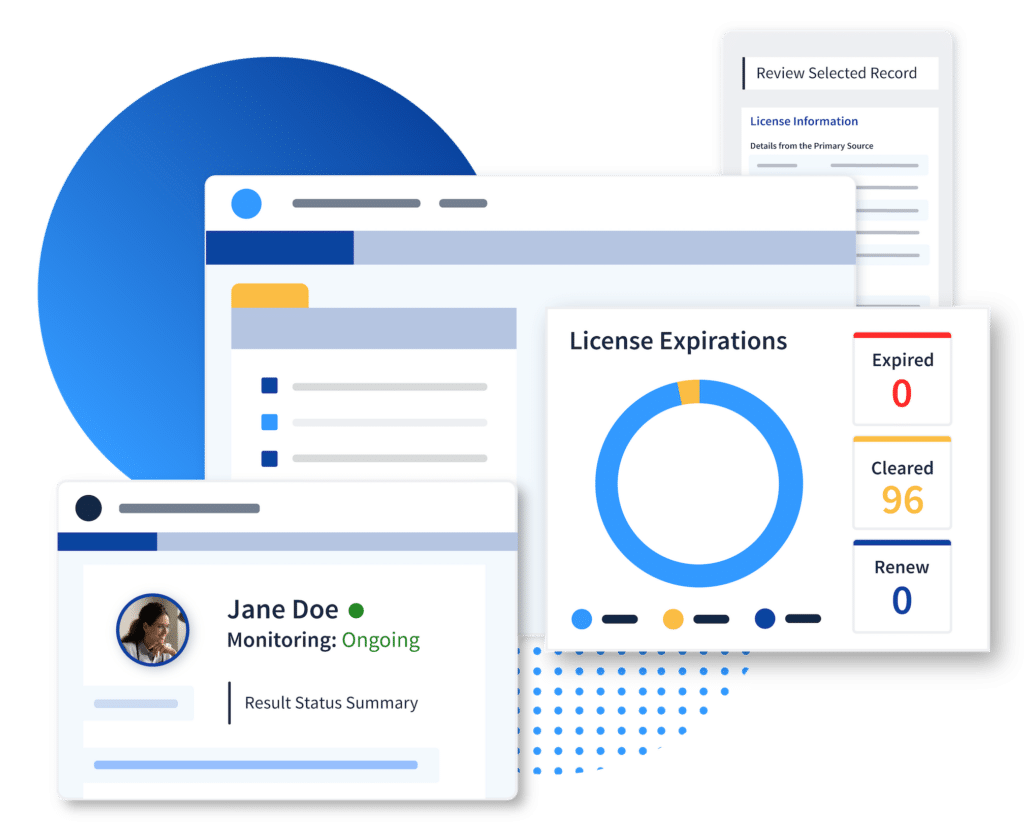
License and Credential Verifications
Go beyond regulatory requirements with ease.

Data Security
Ensure SOC II and NCQA-certified security standards and controls.
Network Accuracy

Reporting and Documentation
Always be audit-ready with primary source documentation for every provider.








