Compliance Monitoring Crafted for HR Confidence
Eliminate administrative complexity often plaguing HR and Compliance workflows, keeping HR teams focused on your organization’s greatest asset – its people.
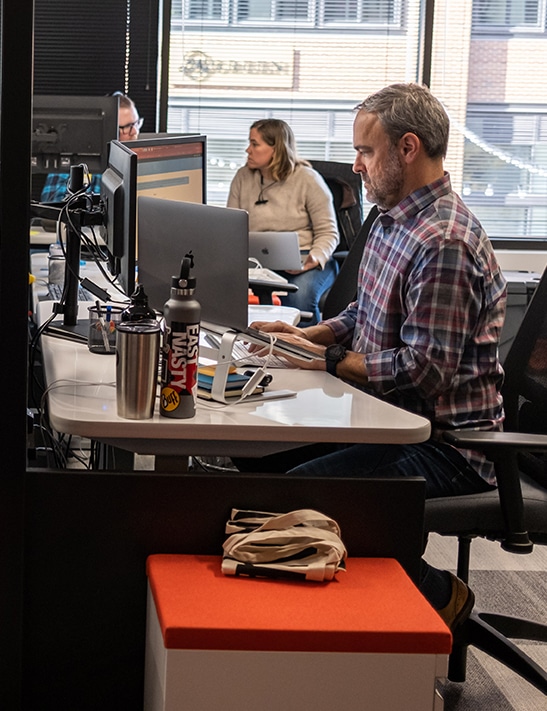
Spend More Time Developing Your People
Don’t let HR administrative complexity keep you from helping your employees grow and succeed. We deliver healthcare’s most trusted ongoing compliance monitoring to ensure continuous compliance across all HR and Compliance requirements.
Distributed Compliance Creates Administrative Complexity
Streamline your process to keep focus on your people
Partnership between HR and Compliance allows for a centralized ownership of processes. We help your teams standardize and simplify the process of compliance monitoring, delivering freedom from your process to focus on your people.
An evolving healthcare landscape leads to licensure challenges
Automated, Ongoing Monitoring of Your Entire Workforce
License and credential verification designed to scale
We verify any potential matches for you
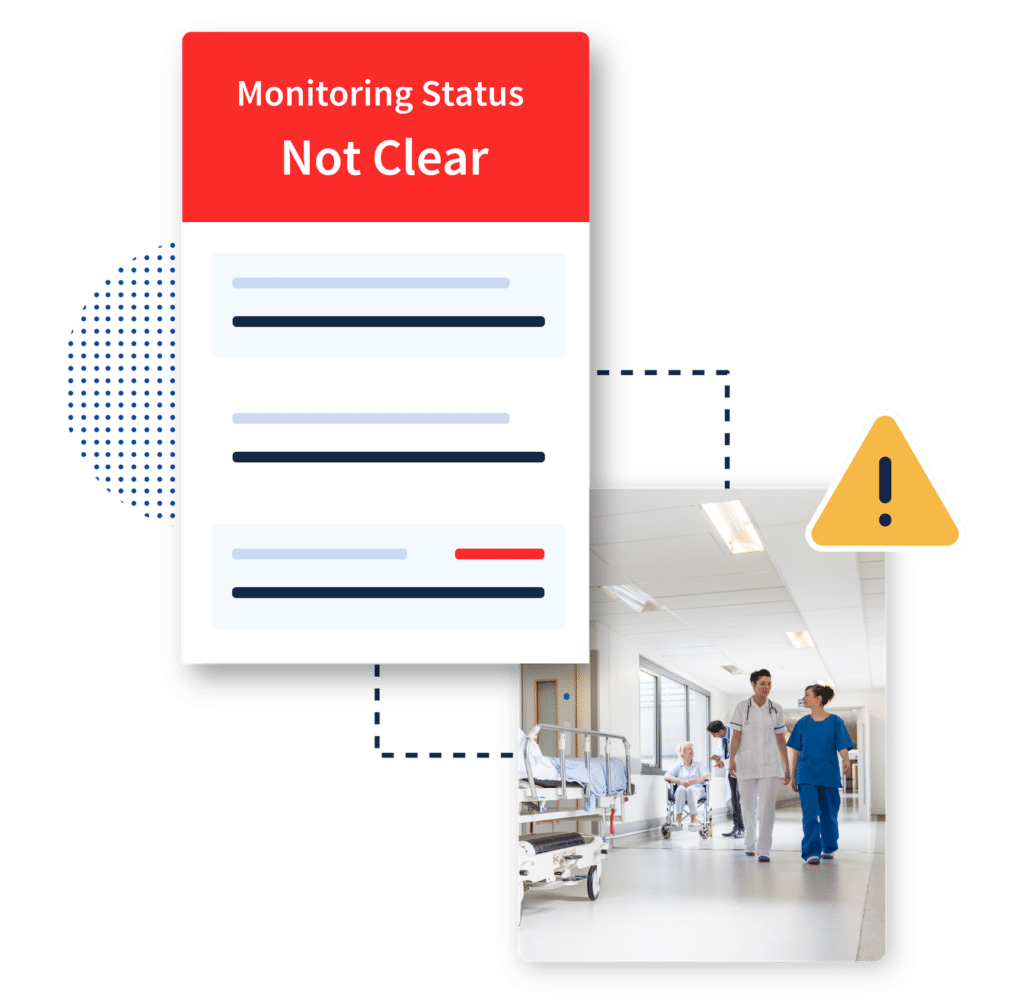
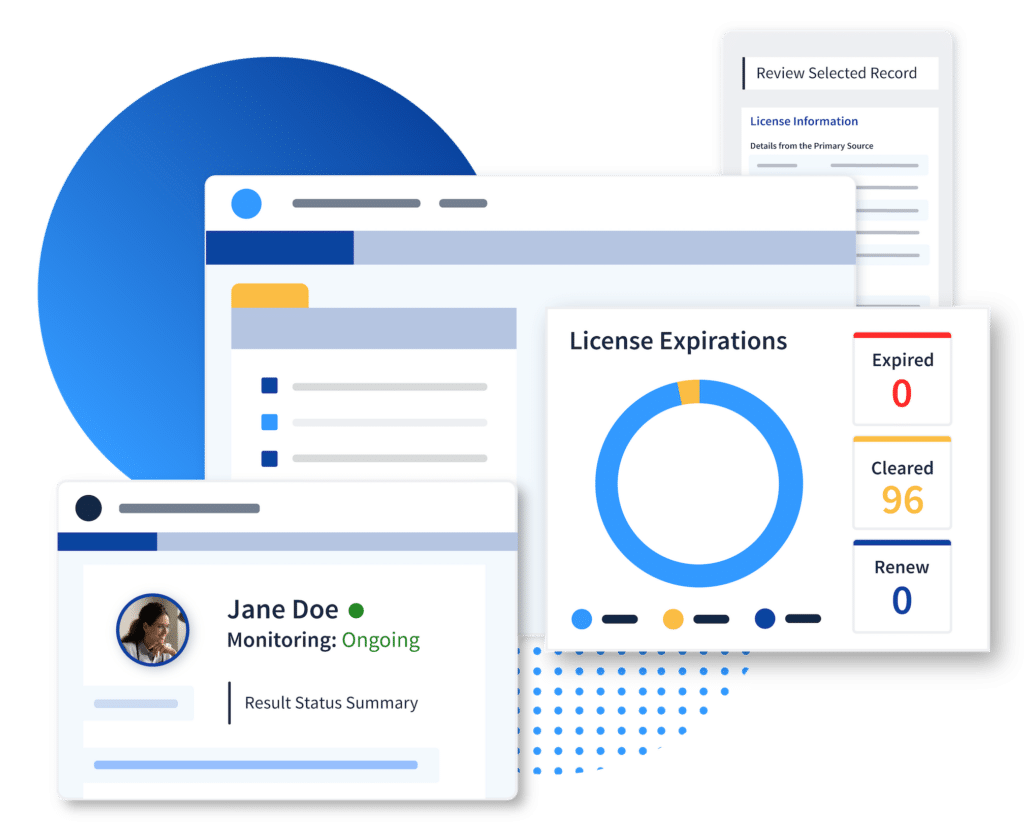
Confidence that Every Care Provider is in Good Standing
Workflow design with prioritization in mind
We’ve engineered dashboards to identify and prioritize potential compliance issues, complete with all the necessary documentation and verification history, for your HR teams to quickly address and resolve.
Securely integrate with your HRIS
Thoughtfully Curated for Your Organization
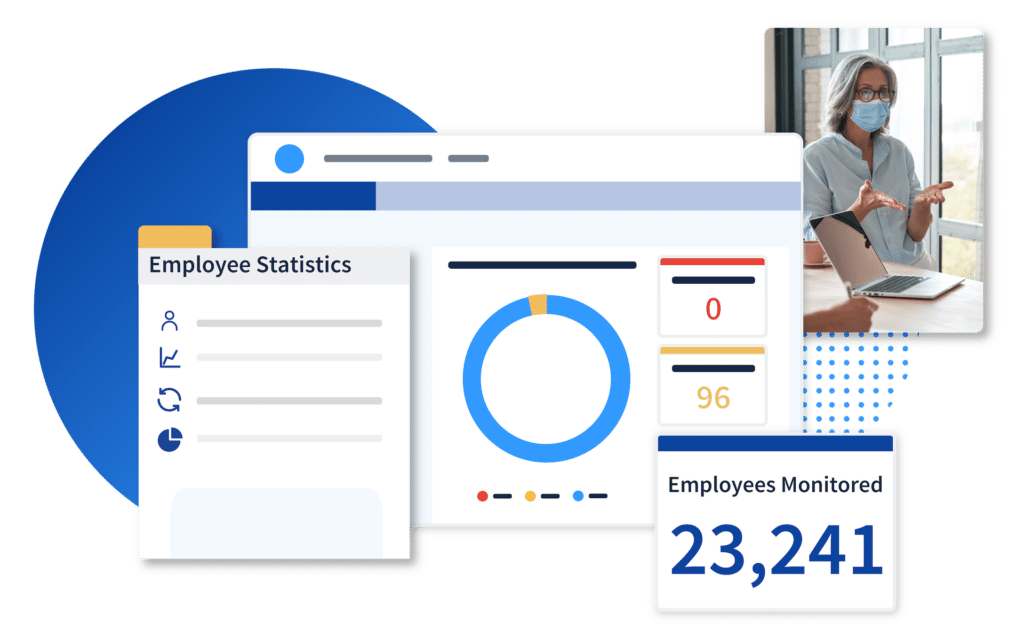
Employee Monitoring
We deliver healthcare’s most trusted ongoing compliance monitoring for every employee.
License and Credential Verifications


“What we've got right now is a place that we can go at any time and look at a point-in-time verification for an employee since ProviderTrust does this quarterly on top of license renewal. I'm able to look at any given time and see a clean PSV, and I'm able to pull that and put it into an employee's file and not stress out because the website for the state is not working today. We've not had issues with things not getting verified.”

“We're in healthcare, and there's high turnover. You don't want to be checking people who aren't here anymore, and you want to make sure you're checking the right people. So that's, again, a comfort to me that we're doing what we're supposed to be doing. At least, what I know of ProviderTrust, that's your focus, and that's what you do. It's not just one of 12 other service lines that someone's trying to sell me. I feel like ProviderTrust has a real focus on providing a cost-effective and efficient service to its clients by concentrating on exclusion checks. Their customer service is excellent!”
Innovated for intelligence. Handcrafted for humans.

Primary Source Verification
Verify every license and credential for all providers directly at the primary source.
Renewals and Expirations

Reporting and Documentation
Always be audit-ready with primary source documentation for every provider.








