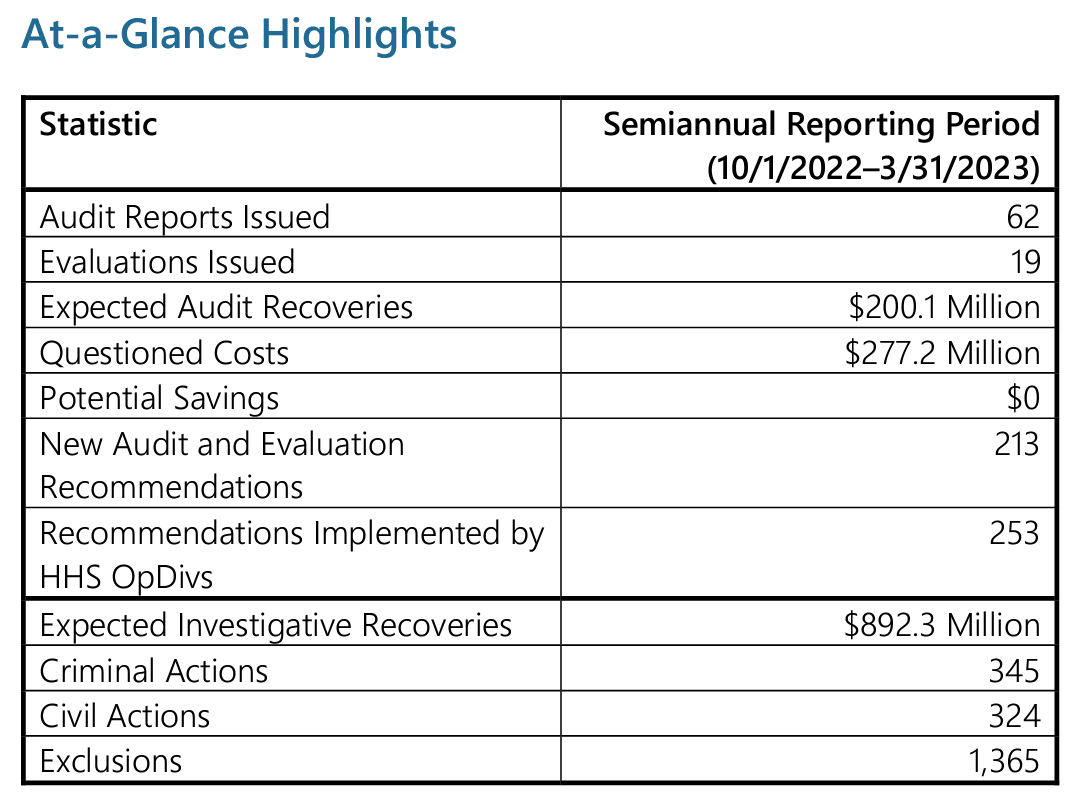
The Department of Health and Human Services (HHS) Office of Inspector General (OIG) has released its latest 2023 Spring Semiannual Report to Congress, providing a comprehensive overview of its activities from October 2022 to March 2023. Led by acting Inspector General Christi A. Grimm, the OIG continues its tireless efforts to uncover instances of fraud, waste, and abuse within HHS programs.
Despite limited resources, the OIG’s work during this reporting period resulted in significant achievements, including 1,365 exclusions, $892.3 million in expected investigative recoveries, 354 criminal actions, and 324 civil actions. This post will delve into the key highlights, focus areas, and accomplishments presented in the semiannual report, shedding light on the OIG’s crucial role in safeguarding the integrity of federal healthcare programs and addressing emerging challenges such as the COVID-19 pandemic.
A Message from Acting Inspector General Christi A. Grimm
Acting HHS-OIG Acting Inspector General Christi A. Grimm submitted the Semiannual Report to Congress summarizing the Department of Health and Human Services (HHS) Office of Inspector General (OIG) activities for the 6-month period ending on March 31, 2023.
OIG continues to work tirelessly to identify instances of fraud, waste, and abuse and prosecute offenders. During this reporting period, its work resulted in 1,365 exclusions, $892.3 million in expected investigative recoveries, 354 criminal and 324 civil actions. This is an increase in exclusions from the last three reporting periods but a decrease in recoveries, criminal and civil actions. This may be due to the limited resources HHS-OIG is currently dealing with.
According to Grimm, “Our capacity to shine a light on program vulnerabilities, uncover misspent funds, and undertake enforcement actions is limited only by our available resources. Notwithstanding concerted efforts by HHS-OIG and the Department — with strong support from Congress for HHS-OIG’s oversight and enforcement — serious fraud, waste, and abuse continue to threaten HHS programs and the people they serve. With current resources, HHS-OIG is unable to keep pace with these threats.”
What is the HHS-OIG Semiannual Report to Congress?
The OIG Semiannual Report to Congress describes OIG’s work on identifying significant problems, abuse, deficiencies, remedies, and investigative outcomes relating to the administration of HHS programs and operations disclosed during the reporting period. In the report, OIG publishes expected recoveries, criminal and civil actions, and other statistics as a result of their work for the semiannual reporting period.
The HHS Office of Inspector General (OIG) has released its latest version of the 2023 Spring Semiannual Report to Congress to summarize OIG activities from October 1, 2022, to March 31, 2023. To reference previous archived reports, visit the OIG Semiannual Reports Archive. Below are some highlights, focus areas, results, and more from HHS-OIG during the reporting period.
HHS-OIG’s Work Plan
Each month, OIG releases their Work Plan updates to inform the public about the projects they are taking on during the year, including auditing, reporting, and investigating HHS operating divisions, including the following:
- Centers for Medicare & Medicaid Services (CMS)
- Public health agencies such as the Centers for Disease Control and Prevention (CDC)
- National Institutes of Health (NIH)
Administration for Children and Families (ACF) - Administration for Community Living (ACL)
- Various state and local governments – evaluate the use of federal funds and the administration of HHS
*Some of the projects described in the Work Plan are statutorily required.
Accomplishments and Excluded Individuals and Entities
The Office of Inspector General (OIG) continues to play a pivotal role in combating fraud within HHS programs and ensuring that wrongdoers are held accountable for their actions. Through collaborative efforts with partners such as the Department of Justice (DOJ), Medicaid Fraud Control Units (MFCUs), and various federal, state, and local law enforcement agencies, the OIG employs a comprehensive and data-driven approach to detect, investigate, and prosecute instances of fraud.
During the reporting period, OIG’s work resulted in expected investigative recoveries of $892.3 million, sending a strong message that fraudulent activities will not go unpunished. Furthermore, the OIG successfully pursued 345 criminal actions and initiated civil actions against 324 individuals and entities found to be engaged in fraudulent practices.
As part of their commitment to safeguarding the integrity of federal healthcare programs, the OIG took decisive action by excluding 1,365 individuals and entities from participating in these programs.
Responding to the COVID-19 Pandemic and Other Emergencies
The Office of Inspector General (OIG) has pursued four primary objectives regarding the Department of Health and Human Services (HHS) response and recovery efforts in relation to COVID-19:
- Safeguarding the well-being of individuals
- Protecting financial resources
- Preserving essential infrastructure
- Enhancing the effectiveness of HHS programs
Although the Public Health Emergency declaration by HHS concluded in May 2023, these four objectives will continue to guide OIG’s strategic planning and execution of its mission in addressing COVID-19.
OIG also remains engaged with federal partners like the Department of Justice (DOJ) to identify and prosecute individuals who exploit the COVID-19 response for their own gain. During this reporting period, an individual was sentenced to three years of probation for fabricating false COVID-19 vaccine records. The convicted individual was employed as a data entry specialist at a vaccination provider company. Their fraudulent activities included creating counterfeit vaccination cards and entering fictitious vaccination records into the Vaccine Administration Management System for 14 individuals.
Leveraging Oversight To Protect Nursing Home Residents Better
Enhancing the quality of care in nursing homes remains paramount to OIG. Through years of oversight, they have discovered various obstacles and weaknesses within nursing home facilities. The COVID-19 pandemic only accentuated the challenges faced by these establishments.
In order to better identify and combat fraud, waste, and abuse and aid policymakers, OIG’s nursing home oversight efforts will adhere to a three-part strategy they call the PRO Framework.
PRO stands for:
- Performance: Facilities should understand what drives nursing home performance, particularly what contributes to poorly performing nursing homes.
- Residents First: Nursing homes should ensure they are promoting high-quality care for their residents.
- Oversight: Entities responsible for nursing home oversight— CMS and individual states— should detect problems quickly and insist on rapid remediation.
OIG currently has 26 ongoing audits and evaluations of nursing home issues, and they continue to monitor areas of concern, push for the implementation of certain recommendations, and issue new guidance as problems are identified and solutions are created.
Promoting Integrity and Effectiveness in Medicare Advantage and Medicaid Managed Care
Almost half of all people covered by Medicare are enrolled in Medicare Advantage organizations, and this trend is expected to continue, with enrollment projected to reach 53% by 2031. In the realm of Medicaid, managed care has emerged as the prevailing payment model. Both state and federal expenditures on Medicaid managed care are steadily increasing, with expenditures totaling $421 billion and representing 59% of all Medicaid expenditures in 2021.
OIG completed the following work related to Medicare Advantage and Medicaid Managed Care during this reporting period:
- CMS Generally Ensured That Medicare Part C and Part D Sponsors Did Not Pay Ineligible Providers for Services to Medicare Beneficiaries
- Keystone First Should Improve Its Procedures for Reviewing Service Requests That Require Prior Authorization
- The Inability To Identify Denied Claims in Medicare Advantage Hinders Fraud Oversight
Sanction Authorities and Other Administrative Actions
During the reporting period, OIG took action to exclude 1,365 individuals and entities from participating in Medicare, Medicaid, and other Federal health care programs. The majority of these exclusions were the outcome of convictions related to Medicare or Medicaid fraud, patient abuse or neglect, financial misconduct, controlled substances, or due to license revocation.
As part of their efforts, OIG successfully implemented a new web-based portal for the Medicaid Fraud Control Units (MFCUs) to report convictions, streamlining the process of imposing exclusions. Additionally, OIG assumes the responsibility of reinstating providers who apply and satisfy the necessary criteria following their exclusions. View the OIG’s Exclusion Database here.
Clearly, fraud continues to be a pervasive problem within the U.S., and the OIG is hyper-focused on auditing, discovering, and pursuing those who commit fraud. The OIG sees its role in protecting the health and welfare of the federal dollars entrusted to HHS and the safe and well-being of those who receive care.