The CMS Preclusion List was released to Medicare Advantage plans and Part D sponsors on January 1, 2019. Since that time, our team has received the provider and prescriber data and began to analyze some of the trends and metrics that can be applied to those who were found on the list.
To help you better prepare for this new requirement, let’s take a look at who the new rule applies to and how to interpret the information provided.
What is the CMS Preclusion List?
The Preclusion List from the Centers for Medicare and Medicaid Services (CMS) is a list of providers and prescribers who are precluded from receiving payment for Medicare Advantage (MA) items and services or Part D drugs furnished or prescribed to Medicare beneficiaries. Starting in January 2019, the Preclusion List from the Centers for Medicare and Medicaid (CMS) is being made available to all Medicare Advantage plans and Part D sponsors, and will officially go into effect in April 2019.
This new rule has been put into action to replace the Medicare Advantage (MA) prescriber enrollment requirements. In addition, the list will be used to ensure patient protection and safety, and protect Trust Funds from prescribers and providers who are identified as fraudulent.
How will the Preclusion List Affect Medicare Advantage (MA) Plans and Part D Prescribers?
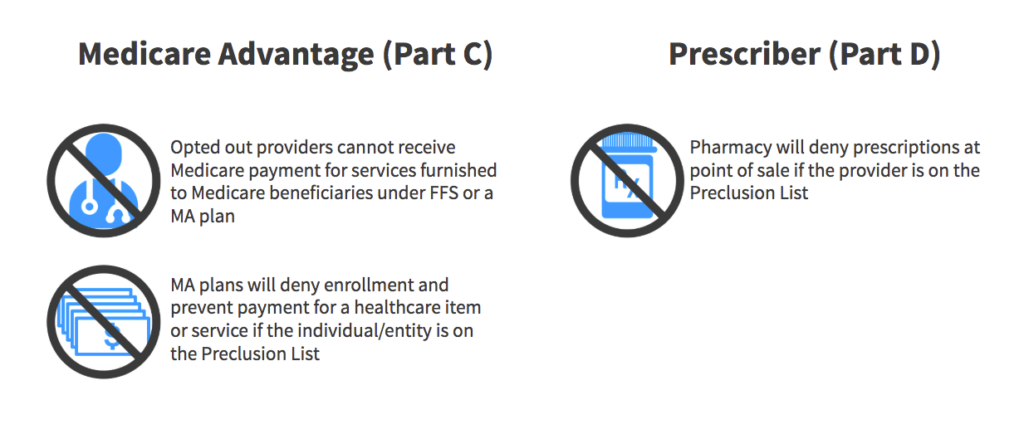
CMS will make the Preclusion List available to Part D sponsors and Medicare Advantage (MA) plans. The initial list of providers will be precluded effective January 1, 2019. MA and Part D plans will not begin editing claims until April 1, 2019. This consists of 30 days for the MA and Part D plans to review the Preclusion List and notify the affected patients by mail if they have received a healthcare item or service or prescription drug in the past from a provider that has been added to the CMS Preclusion List.
The notification will allow a 60-day period before Part D sponsors reject a pharmacy claim (or deny a beneficiary request for reimbursement) for a Part D drug that is prescribed by an individual on the Preclusion List, and MA plans deny payment for a health care item or service furnished by an individual or entity on the Preclusion List.
We recently hosted an educational webinar on what the preclusion list is and how to prepare with Annie H. Shieh, Senior Compliance Counsel for Central Health Plan of California.
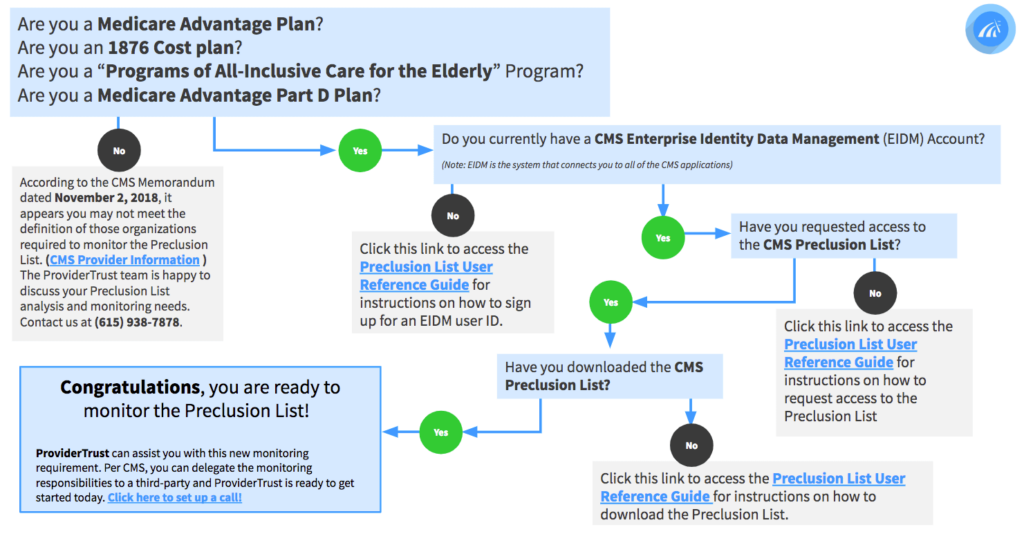
Who Does the CMS Preclusion List Apply To?
The new rule aims to allow more flexibility for healthcare providers and suppliers not currently enrolled in Medicare to provide care to Medicare Advantage (MA) members. Also, providers who have chosen to opt-out of traditional Medicare are able to prescribe with Part D covered drugs or administer care for Part C beneficiaries.
The CMS Preclusion List is not made public for anyone to download, so before creating an account and going through the process to gain access, take a look to see if monitoring this list applies to your organization.
Are the Preclusion List and the OIG Exclusion List the Same?
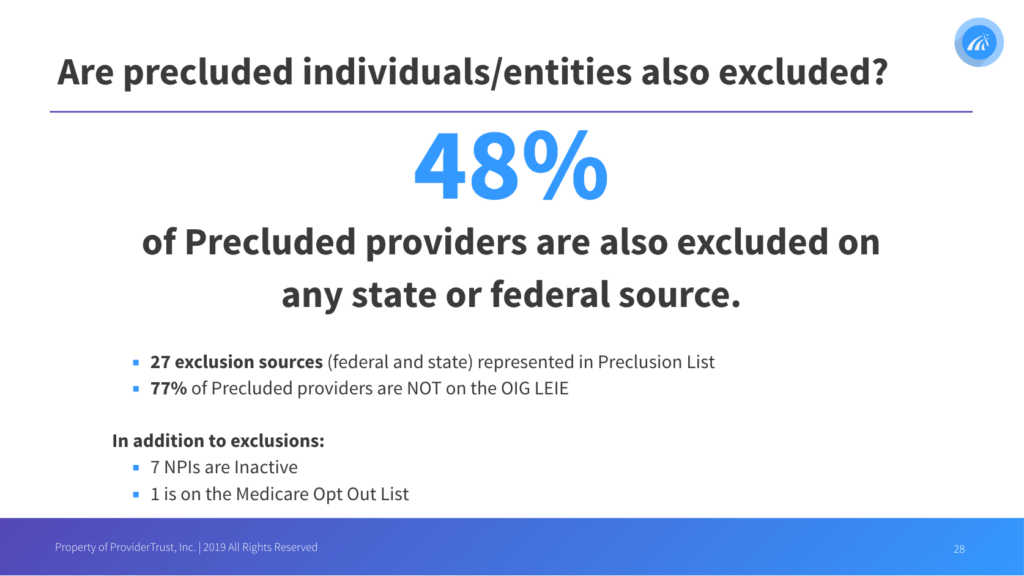
No, healthcare organizations must check the CMS Preclusion list as well as monitor for state and federal exclusions (OIG LEIE, SAM, State Medicaid Lists) or sanctions on an ongoing basis. The Preclusion List does not replace regulatory requirements related to provider selection, credentialing, and oversight under the regulations at §§ 422.204 (MA organizations), 417.416 (1876 Cost Plans) and 460.64 through 460.71 (PACE organizations).
Use of the Preclusion List does not eliminate or address the responsibility for Medicare plans MA and Part D plans to validate that providers are not included on the Office of Inspector General (OIG) exclusion file.
The Preclusion List and exclusion file overlap in the sense that excluded providers will be on the preclusion list but precluded providers who are not excluded will not be on the exclusion file. Therefore, if a plan finds a provider on the OIG exclusion file, the plan is not required to check the Preclusion List.
It is easy for some confusion to set in because of the nature of common healthcare phrases or terms being used in multiple settings, but meaning completely different things. For example, the state exclusion list for Pennsylvania is called, “Pennsylvania Medicheck Precluded Providers List” as well as other instances of providers being considered, “precluded” on certain state exclusion/sanction lists.
Initial Preclusion List Insights
Our data team at ProviderTrust was able to gather some insights from the initial CMS Preclusion List including describing the overlap and differences between various federal lists and the types of healthcare providers or organizations that are found on the new list.
January’s initial list included 1,336 total records, with 618 businesses and 718 individuals named. According to provider specialties, here is how the list was broken down:
TOP 10 Precluded Providers by Specialty
- Clinic / Group Practice – 446
- Internal Medicine – 95
- Family Practice – 94
- Chiropractic – 60
- Nurse Practitioner – 50
- Physician Assistant – 37
- General Practice – 35
- Psychiatry – 30
- Clinical Social Worker – 30
- Home Health Agency – 28
Excluded Providers on the Preclusion List
When comparing our data between exclusion and preclusion lists, 48% of precluded providers were also found to be excluded from any state or federal source (OIG LEIE, SAM.gov, All Medicaid State Lists). Our report also showed that 27 different sources (federal and state) were represented with the overlap between each list. On average, we’ve seen that it takes 173 days for a state exclusion to make it to the OIG LEIE, even though states are required to report within 30 days from HHS OIG. In addition to exclusions, there were a few other stats that stood out to us and overall provider monitoring – 7 NPIs on the list were found Inactive and 1 entity was found on the Medicare Opt-Out List as well.







