The Texas Exclusion list and all state Medicaid exclusion lists are critical components of an effective exclusion monitoring program. With more than 11,000 exclusions, Texas has one of the largest state lists, but the interface makes it a more user-friendly list than many.
In this post, we provide an overview of the Texas Exclusion List, how to screen against it, and a summary of the data it contains.
What is the Texas Exclusion List?
The Texas Health and Human Services (HHS) Commission protects the health and welfare of Texas Medicaid and other HHS program beneficiaries by preventing the participation of excluded individuals and entities. There are many reasons an individual or entity may face exclusion, including convictions for program-related fraud and patient abuse, licensing board actions, HHS and OIG exclusion actions, and “permissive” exclusions, as allowed by certain legal authorities.
Every provider has a responsibility to ensure that items and services furnished by excluded people and entities are not billed to Maternal and Child Health Services (Title V), Medicaid (XIX), Block Grants for Social Services (Title XX), or other HHS programs after the effective date of those parties’ exclusion. This means carefully screening employees and monitoring both federal and state exclusion lists on a regular basis.
For providers in Texas, The List of Excluded Individuals/Entities by the Texas Office of Inspector General (OIG) is the state’s largest exclusion source for all individuals and entities affected by various legal authorities. The Texas exclusion list is available in both text and Excel format, and can be accessed on the OIG’s Texas Health and Human Services page. Updated daily and maintained by OIG, this list contains names and information of all currently excluded parties in Texas, of which there are currently over 11,000.
Individuals and entities excluded from the aforementioned HHS programs may face investigation and a wide range of penalties. First and foremost, excluded individuals will not be reimbursed for any services or items they furnish after the effective date of their exclusion. They also cannot personally—or through a clinic, corporation, or group— bill, request, or receive payment from HHS programs. Excluded individuals also cannot assess care or order or prescribe services to HHS program recipients, regardless of whether these services were provided directly or indirectly.
Besides checking the Texas exclusion list, service providers should also stay up to date on the two main federal exclusion lists, LEIE and SAM. Anyone who hires an individual listed on any of these lists may be subjected to investigation, civil actions, or civil monetary penalties (CMPs). Continually monitoring both state and federal exclusion lists is the best way to eliminate fraud in your health ecosystem.
Who needs to monitor the Texas OIG Exclusion List?
If your organization participates in federal healthcare programs (Medicare, Medicaid, CHIP, VA), either by directly furnishing goods or services or indirectly, but working with a healthcare provider, then you need to monitor the Texas OIG exclusion list.
Screening your healthcare populations against Medicaid exclusions is not only one of the most valuable defenses in protecting your organization and patients, but they also ensure the integrity of healthcare dollars. To ensure that healthcare employees are not on any exclusion lists, Medicaid providers must regularly screen all of their employees (from pre-employment and on an ongoing basis).
Organizations that employ or conduct business with an excluded provider may be subject to Civil Monetary Penalties (CMPs). CMPs enforced by HHS OIG or false claim allegations by the U.S. Department of Justice (DOJ) can result in more than $20,000 per false claim or statement, plus treble damages. Here are the latest CMPs published by the OIG.
How do I check the Texas Exclusion List?
To search the Texas Exclusion List, visit the Office of Inspector General’s website. Unlike some state lists where you can download a spreadsheet, the Texas Exclusion List has an interactive search function that allows you to manually search up to five individuals or company names simultaneously.
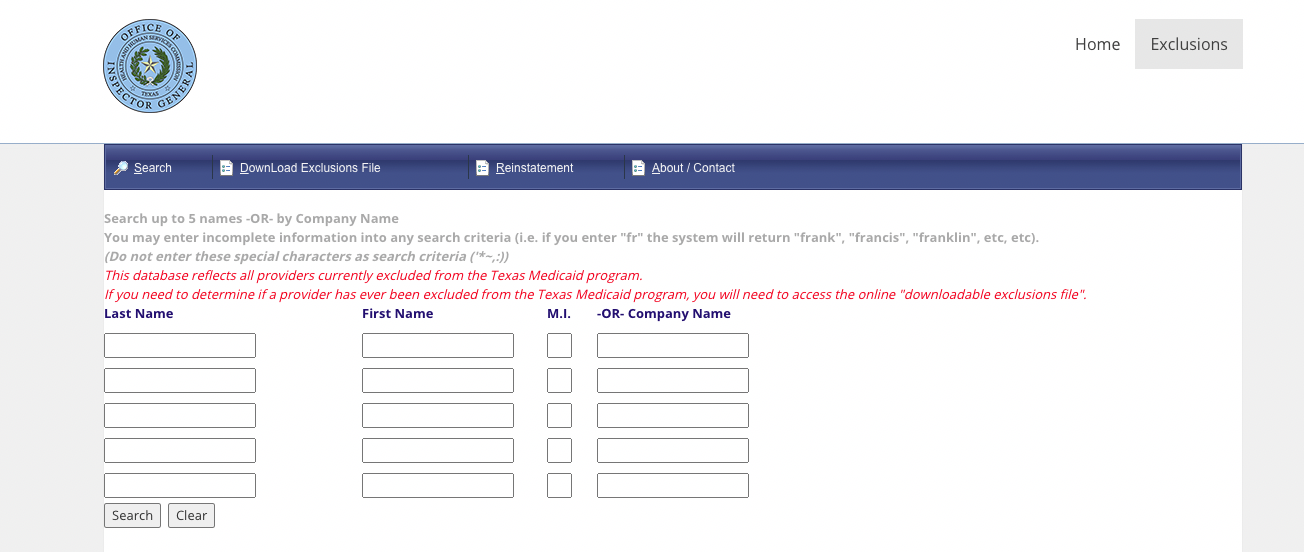
If you wish to identify if a provider was ever excluded from the Medicaid list (not a current exclusion), you will need to access the online downloadable exclusions file.
Identifying Matches on the Texas Exclusion List
When you’re trying to confirm whether an individual or entity appearing on the Texas exclusion list is, in fact, the same one within your population, you must confirm such a match based on uniquely identifying data points (not just a name or address). ProviderTrust’s best-in-class data enrichment strategy catches and verifies issues no one else can, alerting you to exclusions you would never otherwise find.
Data Completeness
When it comes to any exclusion list, data completeness is always a challenge. Within the Texas exclusion list, we find:
- 76% have a license number
- 4% have a National Provider Identifier (NPI)
- 0% have a DOB
- 0% have addresses, city, or state information
Because high-confidence, high-quality exclusion matches are only possible by matching uniquely identifying data (such as a SSN or NPI), it can be difficult and time-consuming to manually confirm Texas exclusions and catch bad actors who may be using a different name or license.
How Texas Compares to States Nearby
The industry standard is to monitor healthcare populations (employees, providers, vendors) against all federal and state exclusion lists on an ongoing basis. Each month, we update our Exclusion Map with data from all federal and state exclusion or terminated provider lists for easy reference. Here’s a snapshot of the states surrounding Texas:
- New Mexico and Oklahoma don’t have state exclusion lists
- Louisiana has DOB, SSN verification, and 6% NPI reported
- Arkansas has city, state, and zip code only
Reporting Timeline
When reviewing state exclusion lists, you’ll see that they’re all updated differently. While some are not updated regularly, others, such as the Texas Exclusion List, are updated continuously. Although there is no set update schedule, ProviderTrust regularly aggregates and enriches the latest primary source data to ensure our dataset remains more complete than most primary sources.
Texas Exclusion List FAQ
The New Standard for Exclusion Monitoring
At ProviderTrust, we deliver healthcare’s most trusted ongoing state and federal Medicaid exclusion list monitoring, thoughtfully engineered for every unique population. Our exclusion monitoring solution is fully automated – we can screen your employees, providers, and vendors against every state and federal exclusion source up-to-daily. From OIG exclusions to licenses and credentials, our healthcare monitoring and verification platform goes beyond good enough.









