The Industry's Most Trusted Exclusion List Monitoring
Leveraging Best-in-Class Data for Unbeatable Accuracy
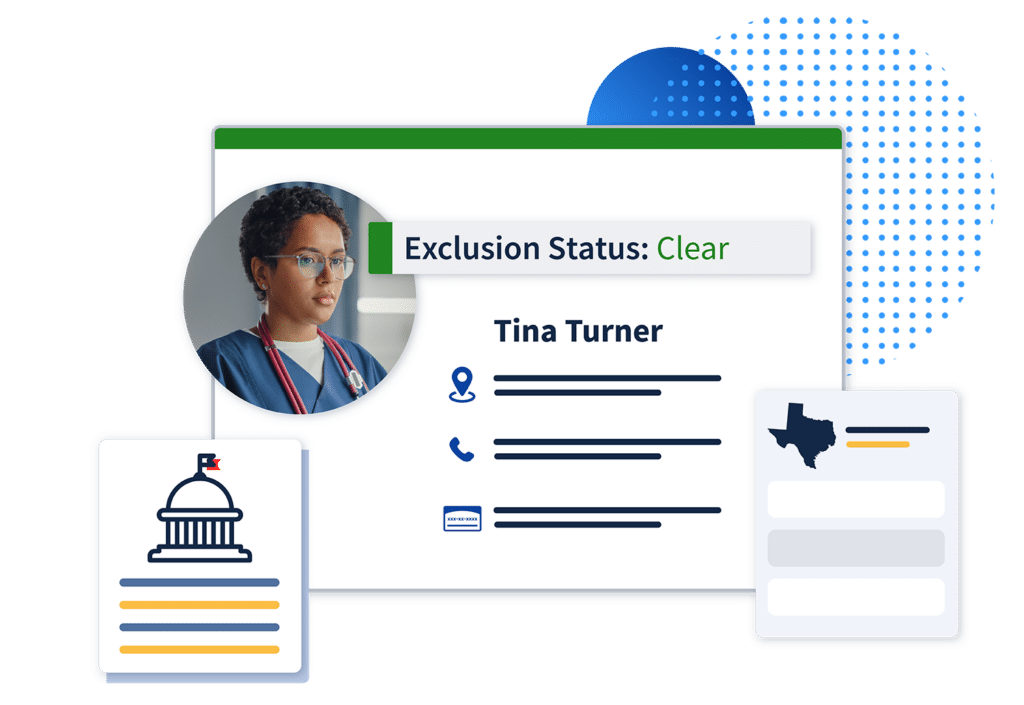
Prioritize Your Data Integrity
Since our founding in 2010, ProviderTrust has continued to evolve our industry-leading automated exclusion monitoring to make healthcare safer and more equitable. Reduce your risk and protect patients while removing time-consuming manual work from your team with NCQA-certified ongoing coverage that delivers exact-match results only.
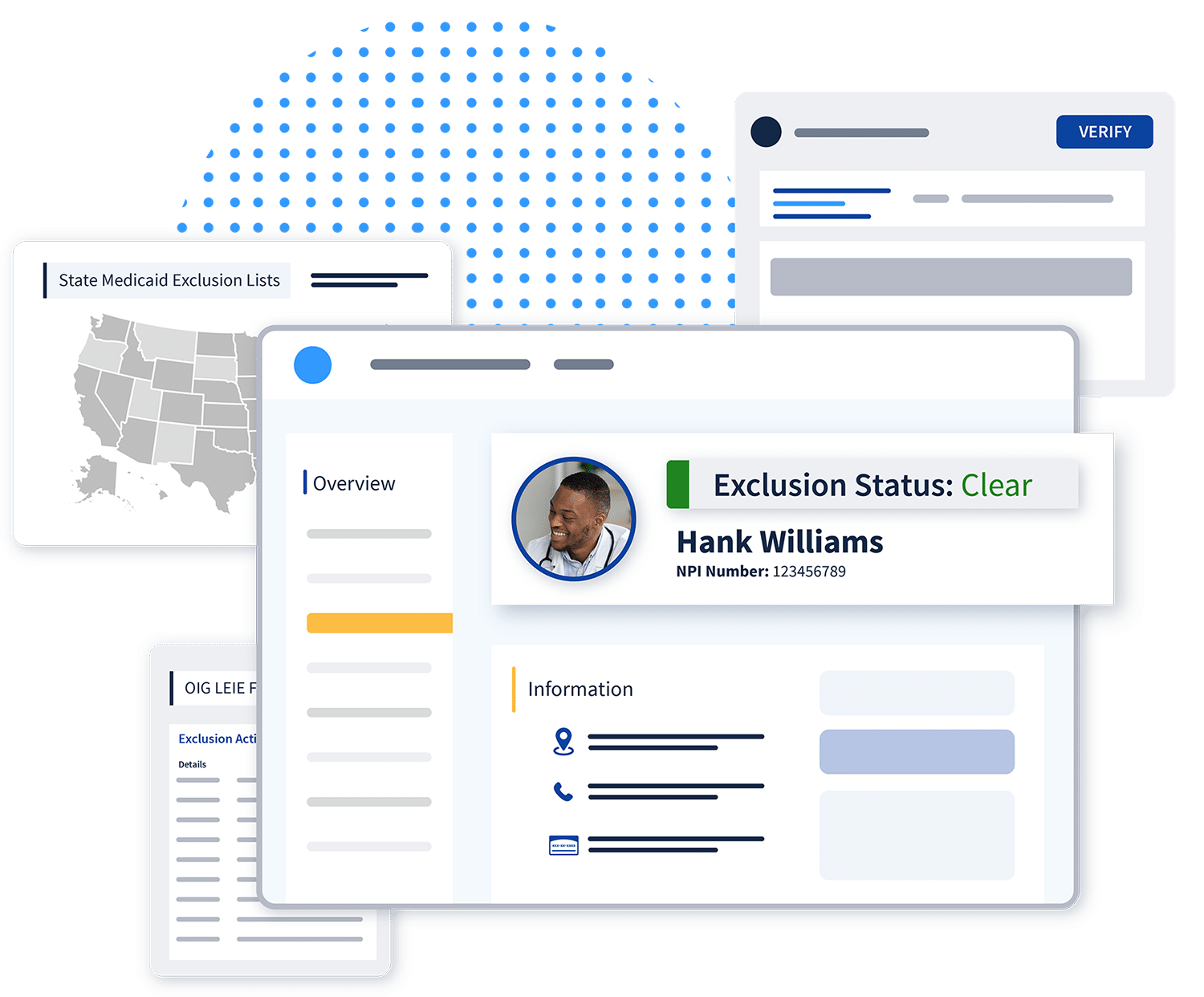
From the moment we turn on exclusion monitoring, your data becomes better than the primary source. How? We create a custom dataset with unbeatable accuracy by enhancing primary source data and your own data with unique identifiers to deliver faster, more reliable results. Our data makes a difference—51% of the exclusions we catch are likely missed by other vendors.
Who We Monitor:
- Licensed and non-licensed employees
- Ordering and referring physicians
- Contracted physicians
- Vendors
Fully Automated for Continuous Coverage
Ongoing exclusion checks for all employees
Monitoring for all federal and state exclusion lists
Stay completely covered with continuous screening for:
- HHS-OIG List of Excluded Individuals and Entities (LEIE)
- GSA SAM.gov
- NPPES NPI Registry
- OFAC SDN and Non-SDN List
- Medicare Opt Out
- SSN Death Master File
- CMS Preclusion List
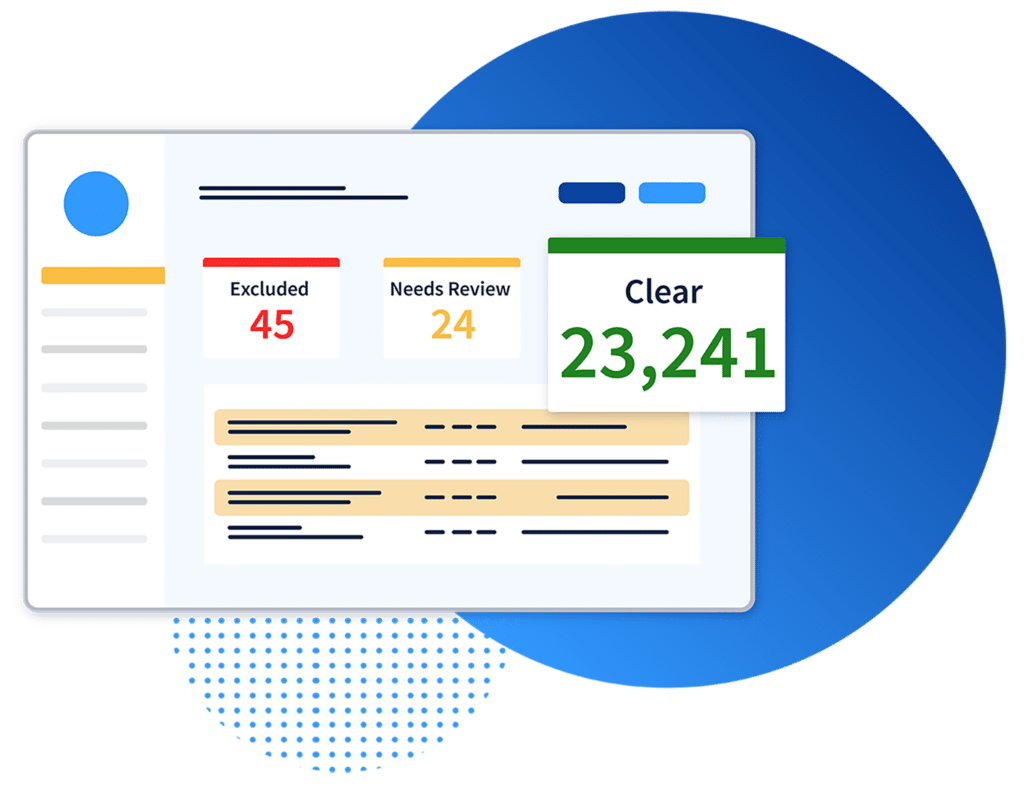
More Reliable Results in Less Time
Data that’s better than the primary source
Exact-match results every time
A Trusted, Secure Solution
Prioritize data security and privacy
Stay audit-ready with detailed reporting
For Compliance Leaders
Impact Compliance™
Together, we can impact change.
Introducing the industry’s highest standards in healthcare compliance monitoring. This comprehensive program provides organizations across the care continuum with a roadmap to implement above-average compliance practices by:
- Addressing key population monitoring gaps
- Prioritizing financial efficiencies
- Upholding community healthcare and success




“Not only has ProviderTrust saved us countless hours of unnecessary work and delivered peace of mind that no exclusions will be missed, but their solution is also the most polished one that we work with and we are frequently complimented on how organized our credentialing files and programs are.”

“Most healthcare companies know how to check the OIG website, but checking all the state Medicaid sites, SSDMF, and all other sources is where ProviderTrust really provides us a great service.”
Integrate Your Applications with ProviderTrust